Infertility affects millions of would-be parents worldwide. The Centers for Disease Control and Prevention (CDC) estimates that around 13 percent of women aged 15–49 in the United States have difficulty getting or staying pregnant. This issue is not limited to women, as male infertility accounts for approximately half of all infertility cases. Modern reproductive medicine also is expanding to address the needs of LGBTQ+ communities as well as individuals opting for single parenthood.
These infertility trends underpin a growing demand for reproductive health specialists to meet the diverse needs of those looking to start or grow their family. Two key players making a difference in this field are embryologists and andrologists — health care professionals whose specialized skills help shape the future of reproductive health.
Explore how embryologists and andrologists impact reproductive medicine, the skills required to excel in these fields, and the pathways for health care providers to advance in these areas.
The growing need for specialists in reproductive medicine
“As the demand for in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) continues to rise, the need for trained embryologists and andrologists will also increase, making these careers a solid choice for individuals interested in reproductive science,” says Marcia Firmani, PhD, MSPH, MT(ASCP), MBCM chair of the Department of Biomedical Laboratory Sciences and Associate Professor and director of the Program in Medical Laboratory Sciences.
These professionals are at the forefront of Assisted Reproductive Technology (ART), contributing to breakthroughs in reproductive health and transforming lives.
Common types of ART procedures include:
- Intrauterine insemination (IUI): Also called artificial insemination, IUI involves placing sperm directly into the uterus around the time of ovulation to increase the chances of fertilization.
- In vitro fertilization (IVF): The most well-known ART procedure, IVF involves retrieving eggs from the ovaries, fertilizing them with sperm in a lab, and then transferring the resulting embryo(s) to the uterus. IVF is often used in cases of severe infertility or when other fertility treatments have failed.
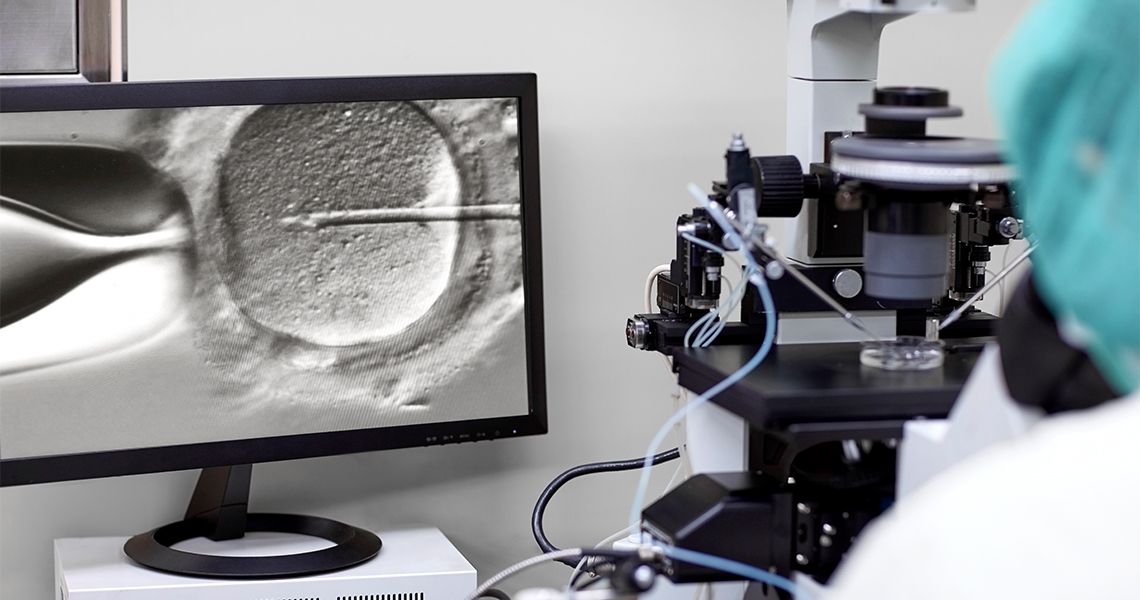
- Intracytoplasmic sperm injection (ICSI): Often combined with IVF, ICSI involves injecting a single sperm directly into an egg to facilitate fertilization. It’s commonly used when there are issues with sperm quality or quantity.
- Frozen embryo transfer (FET): This involves thawing previously frozen embryos (from a previous IVF cycle, for instance) and transferring them to the uterus. FET allows patients to attempt pregnancy without undergoing another round of egg retrieval.
- Egg and sperm donation: Donor eggs or sperm are used in IVF when one partner has low-quality or non-viable eggs or sperm. The donated egg or sperm is combined with the partner's gamete or another donor's gamete, and the resulting embryo is transferred to the recipient’s uterus.
- Gestational surrogacy: In this process, a gestational carrier (surrogate) carries and delivers a child for another person or couple. The embryo is created through IVF and transferred to the surrogate’s uterus, meaning the surrogate has no genetic connection to the child.
- Cryopreservation: This process involves freezing and storing eggs, sperm, or embryos for future use. This method offers individuals and couples the opportunity to conceive at a later time, safeguarding their fertility against age, medical treatments, or life circumstances that may impact their ability to have biological children.
Understanding the role of embryologists and andrologists
Embryologists are the experts behind the scenes in fertility labs. They handle the complex processes of preparing eggs and sperm for fertilization, culturing embryos, and ensuring the quality of each step in ART procedures.
Their work in embryo grading, cryopreservation, and micromanipulation of gametes is essential to the IVF process. By carefully monitoring and cultivating embryos, embryologists play an important role in helping increase the chances of successful pregnancies for hopeful parents.
Andrologists, on the other hand, specialize in male reproductive health. They conduct sperm analysis, perform diagnostic testing, and are responsible for procedures to support male fertility. Andrologists help diagnose and treat conditions such as low sperm count, motility issues, and hormonal imbalances that may be barriers to conception. In a field where male infertility has historically been overlooked, andrologists’ contributions are crucial to comprehensive fertility care.
How embryologists and andrologists contribute to improved patient outcomes
Embryologist and andrologist expertise translate directly to better patient outcomes. The skills and knowledge provided by these specialists help improve the success rates of IVF and other fertility treatments, offering patients hope and increasing the likelihood of successful pregnancies.
Impact on success rates
By working closely with fertility specialists, embryologists contribute to significant improvements in ART outcomes. Through meticulous embryo handling and grading, for instance, embryologists can select the healthiest embryos for implantation, increasing the chance of successful pregnancy. Similarly, andrologists enhance outcomes by identifying male-specific infertility issues that may have gone undetected, enabling personalized treatment plans.
Example scenario: Consider a couple experiencing unexplained infertility after years of trying to conceive. An andrologist conducts a detailed sperm analysis and identifies a motility issue — or an inability of the sperm to move independently — that traditional testing had missed. With this insight, the andrologist recommends specific treatments, and an embryologist then facilitates IVF with ICSI, ultimately leading to a successful pregnancy.
Cases such as this demonstrate how these professionals’ specialized knowledge and hands-on expertise directly impact patient success stories.
Career outlook for reproductive health specialists
According to the U.S. Bureau of Labor Statistics (BLS), jobs for clinical laboratory technologists, including those in reproductive medicine, are expected to grow by 5% from 2023 to 2033. This growth is fueled by advancements in ART technologies, delayed parenthood, and increased awareness of fertility treatments.
The earning potential for reproductive health specialists will vary depending on position, experience, geographic location, and the clinic or hospital where they work. The average salary for embryology and andrology specialists in the United States is between $66,000 and $93,500,000 annually, with experienced embryologists or those in management earning up to $100,000 to $122,000 annually.
How to become a reproductive health specialist
As the demand for reproductive health specialists rises, pursuing further education in these fields is an excellent path for health care providers aiming to contribute meaningfully to the future of fertility medicine.
For those interested in pursuing a career in embryology or andrology, the path involves focused education, training, and experience in reproductive health sciences. Here is a general overview of the steps you can expect:
- Earn a bachelor’s degree: You’ll need to start by earning a bachelor’s degree in a related field, such as biology, biochemistry, or a related life sciences field. If you’re looking for a highly-specialized program, the George Washington University School of Medicine and Health Sciences (GW SMHS) BSHS in Clinical Embryology and Assisted Reproductive Technology (CEART) is the nation’s only bachelor’s degree tailored to assisted reproductive technology (ART).
- Pursue specialized education: Those who earned a bachelor’s degree in a related field will need to obtain additional training specific to the field. The GW SMHS Post-Baccalaureate Certificate in Clinical Embryology is a great option for individuals looking to build onto their existing education or change careers from other health-related specialties.
- Gain hands-on laboratory experience: Many programs, including the ones at GW SMHS, provide opportunities for lab work, where students develop skills in embryo culture, micromanipulation, sperm analysis, and cryopreservation. These skills are critical to success in fertility labs, so having firsthand experience in an educational setting is vital.
- Consider certification options: Although not required, taking the initiative to obtain a certification can enhance job prospects and demonstrate your expertise in the field. GW SMHS students who complete the bachelor’s or certificate programs are eligible to sit for the American Association of Bioanalysts board of certification exams in both embryology and andrology.
- Begin working in a clinic or research facility: After completing your education and training, you can start your career as a reproductive health specialist. Job settings could include IVF labs, fertility clinics, biotechnology companies, or research institutes.
Launch a meaningful career as a reproductive health specialist
Embryologists and andrologists are key players in overcoming infertility, offering expertise that can make a life-changing difference for families. By developing specialized skills, health care providers can contribute meaningfully to this field, supporting families, and advancing reproductive health.
If you’re ready to begin a rewarding career as a reproductive health specialist, learn more about why George Washington University School of Medicine and Health Sciences is recognized for excellence in this growing field. Explore our programs today: